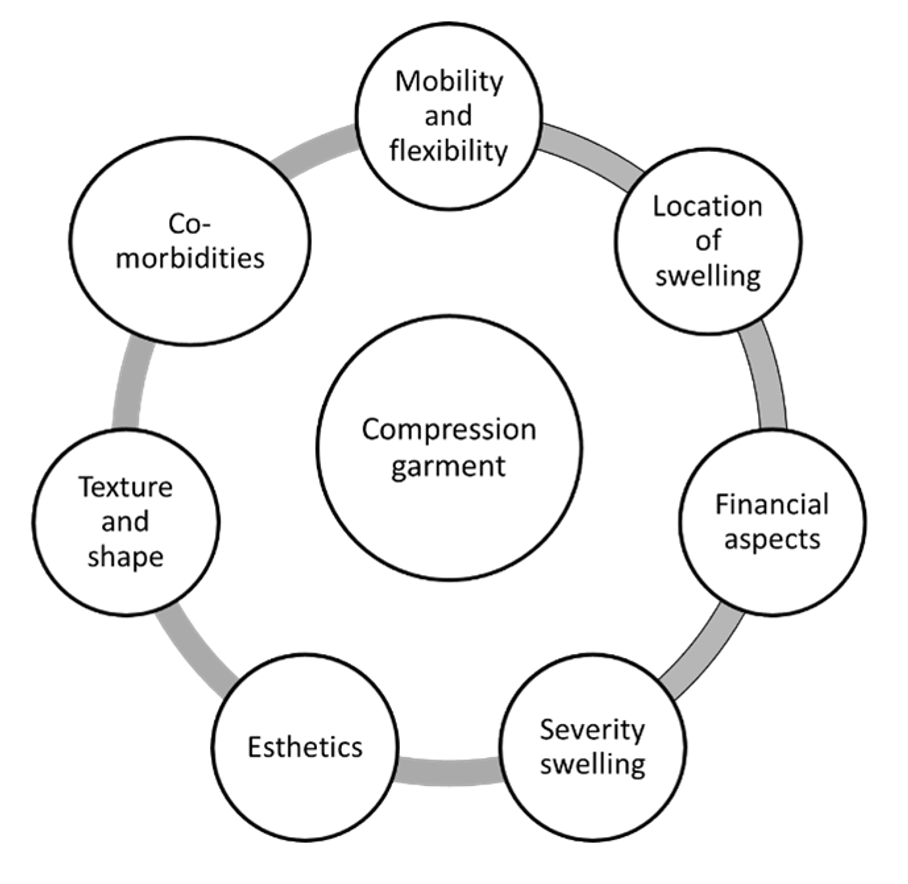
Compression therapy is the cornerstone in lymphedema treatment to reduce and stabilize the swelling of the affected areas. During the intensive phase multilayer bandages are applied to reduce the swelling, while during the maintenance phase these bandages are replaced by compression garments to maintain this reduction.(1) However, not every compression garment can serve this purpose. Therefore, finding the right compression garment is important. There are a lot of aspects to take into consideration (fig.1) and a lot of decisions to make (fig.2). This can be quit overwhelming, but don’t worry, in this blogpost we will try to explain the important aspects to take in consideration when finding your ideal compression garments.
Figure 1
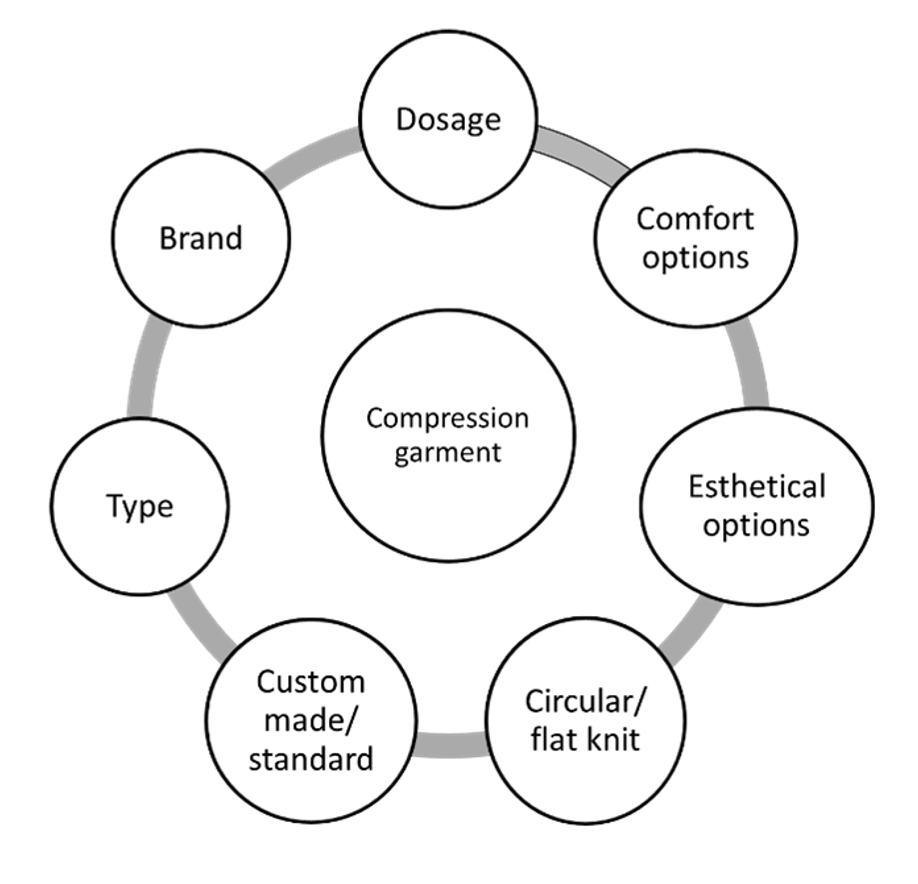
Figure 2
First, it might be important to explain the difference between a circular and flat knit compression garment. A circular knit garment has no seam. To make different sizes, different cylinders with different diameters are being used. Most of these compression garments have standard sizes and are not custom-made. The material is often thinner. Flat knit garments do have a seam and are often custom-made and consist of thicker material.
When choosing the right compression garment, it is first of all very important to get personal advice and treatment from caregivers specialized in lymphedema. (2) A qualified physician should prescribe the compression garment (1), while a compression specialist should measure the compression hosiery.
However, a patient should be involved in this decision-making and therefore it is very useful to understand different principles. Bjork et al. wrote a very interesting article about an algorithm which helps you in the selection of the right compression garment for lower limb edema.(3) This algorithm is called ‘S.T.R.I.D.E’ and takes into account both compression- and patient-specific characteristics(3)
This S.T.R.I.D.E principle gives you an idea of which dosage, stiffness, and length the compression garment should have, as well as it should be flat or circular knit and custom-made or standard.
Shape:
The first thing you should look at is the location of the swelling. The swollen parts should be covered by the compression garment. For example, someone who has a swollen lower leg should have at least a compression garment from the foot until the knee. Don’t forget to look if, for example, the genital region or the toes are involved.
Furthermore, the shape of the limb should be taken into consideration. If the shape of the limb doesn’t match with the shape of the standard compression garment, a custom-made compression hosiery should be measured. The compression specialist should take a look if the circumference of the limb matches the sizing chart of the standardized compression garment. If this is not the case, a custom-made compression hosiery should be chosen. The sizing charts differ between different products and manufacturers, so if there isn’t a match with one product maybe there is a match with another.
Texture:
Depending on the texture of the skin and subcutaneous tissue another type of compression garment needs to be provided. You probably already heard about the pressure/dosage of a compression garment, but actually the stiffness of a compression garment is also an important dynamic property for its effectiveness.(4-7) It differs between products and brands(4) and also depends on the amount of layers(8). More reduction in edema and better haemodynamic parameters are seen with a higher stiffness.(6, 9-13)
If the texture of the tissue is softer and pliable and if your thumb leaves a depression in the skin, a circular knit garment at a lower dosage could be sufficient after bandaging. However, a stiffer circular or flat knit garment might be needed to prevent the garment from creasing into the joint. If the depression in the skin stays in place for >30 seconds after deep and firm pressure and the skin is more difficult to lift, this means there are early fibrotic changes. In this case, stiffer garments are needed to stabilize the edema after bandaging, typically day and night. As the fibrotic changes advance, the skin becomes firmer and it is possible that you cannot see a pit when pressing your thumb into the skin. This requires stiffer garments with a higher dosage during the day and night. Texture in the compression garment could also help to soften the fibrotic tissue.
You should also consider the fragility of the skin. In case of a thin and fragile skin, friction should be minimized by using donning and doffing devices, considering double covered inlay yarns and using an underliner.
In case there is also some abnormal fatty tissue like in lipoedema, a stiffer flatknit garment could be considered to better prevent the garment from cutting into the present creases.
Refill:
The refill gives an indication of when compression should be applied. In case the edema increases only during the day but decreases overnight or with elevation, wearing the compression garment during the day should be sufficient. If, however, the edema also increases during the night, night-time compression should be provided. If the swelling increases fast after removing the compression garment strict adherence to compression and a treatment plan in case of an increase is needed.
Issues:
There are a lot of issues which could influence the result and choice of the compression therapy, like comorbidities, esthetic aspects, physical status, the ability to put on and pull of the compression garment, financial aspects and the support network. A compression garment which is ideal for a certain type of edema isn’t always the best if you look at the bigger picture.
Dosage:
Solely based on the diagnosis, edema at the lower limb requires a dosage of 14-60 mmHg. The more severe the edema is, the higher the dosage must be. (14) However, this doesn’t take into account important comorbidities like peripheral arterial disease, reimbursement, patients’ ability to put on and pull of the compression garment. Sometimes it is also an option to combine two compression garments with a lower dosage to have more stiffness.
Etiology:
The S.T.R.I.D.E principle can be applied on different types of edema, it could also be interesting to take a look at the cause (etiology) of the edema and the contributing factors as these have their own characteristics. For example, edema as a consequence of chronic kidney disease can fluctuate before and after dialysis. In this case an adjustable garment might be needed.
Besides this S.T.R.I.D.E principle, there are other characteristics that should be considered. If the compression garment tends to slide down, some adaptations could be made like a broader silicon band (if you are not allergic to it), another pattern of the silicone, a double silicone band and compression pants. Furthermore, the compression garment could cause some redness or painful spots at the joints. In a custom-made garment some comfort zones could be applied at these painful joints. Also, some pockets could be made to put in a material with structure for the more fibrotic parts for example. Finally, many brands also consider the esthetical part. You can often choose between different colors and prints.
As you noticed compression therapy is not a “one size fits all”. At the beginning it is often difficult to find a good compression garment. Hopefully, the S.T.R.I.D.E principle, the other tips and your compression specialists will help you finding the right one. Discuss problems with your compression specialists, so they can help and guide you to find the one compression garment that suits you or your patient the best. You have to know that it can take time to find good compression garments for a specific patient, but … never give up!
An-Kathleen Heroes
1. Damstra RJ, Halk AB. The Dutch lymphedema guidelines based on the International Classification of Functioning, Disability, and Health and the chronic care model. J Vasc Surg Venous Lymphat Disord. 2017;5(5):756-65.
2. The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology. 2020;53(1):3-19.
3. Bjork R, Ehmann S. S.T.R.I.D.E. Professional Guide to Compression Garment Selection for the Lower Extremity. J Wound Care. 2019;28(Sup6a):1-44.
4. Hirai M, Iwata H, Ishibashi H, Ota T, Nakamura H. Interface pressure and stiffness of various elastic stockings during posture changes and exercise. Vascular. 2008;16(2):95-100.
5. Hirai M, Niimi K, Iwata H, Sugimoto I, Ishibashi H, Ota T, et al. Comparison of stiffness and interface pressure during rest and exercise among various arm sleeves. Phlebology. 2010;25(4):196-200.
6. van der Wegen-Franken CP, Mulder P, Tank B, Neumann HA. Variation in the dynamic stiffness index of different types of medical elastic compression stockings. Phlebology. 2008;23(2):77-84.
7. Partsch H, Clark M, Bassez S, Benigni JP, Becker F, Blazek V, et al. Measurement of lower leg compression in vivo: recommendations for the performance of measurements of interface pressure and stiffness: consensus statement. Dermatol Surg. 2006;32(2):224-32; discussion 33.
8. Hirai M, Koyama A, Miyazaki K, Iwata H, Kominami Y. Interface pressure and stiffness in different combinations of compression material. Phlebology. 2012;27(2):82-9.
9. Häfner HM JM. The Haemodynamic efficacy of six different compression stock-ings from compression class 2 in patients suffering from chronic venous insufficiency. Phlebology: The Journal of Venous Disease. 2000;15(3-4):126-30.
10. Mosti G. Stiffness of compression devices. Veins and Lymphatics. 2013;2(1):1-2.
11. van Geest AJ, Veraart JC, Nelemans P, Neumann HA. The effect of medical elastic compression stockings with different slope values on edema. Measurements underneath three different types of stockings. Dermatol Surg. 2000;26(3):244-7.
12. van der Wegen-Franken K, Roest W, Tank B, Neumann M. Calculating the pressure and the stiffness in three different categories of class II medical elastic compression stockings. Dermatol Surg. 2006;32(2):216-23.
13. Melhuish JM, Clark M, Williams R, Harding KG. The physics of sub-bandage pressure measurement. J Wound Care. 2000;9(7):308-10.
14. framework L. Best practice for the management of lymphedema. International Consensus. 2006.