The puzzle called pain.
Pain, it is something that almost all of us experience on a daily basis. You stub your big toe against the leg of the chair and yell “ouch”. Unfortunately, 20% of the world's population experiences persistent pain without even bumping their toe against a chair. The question why these people are in pain has a very complex answer, or maybe we don’t really have an answer. Read on to find out more!
What is pain?
In a nutshell: Pain is an unpleasant sensory and emotional experience associated with actual (wound) or potential tissue damage (punch of the aforementioned toe). Moreover, the nervous system (the nerves in your limbs, your spinal cord and your brain) is always involved in such pain experiences and is influenced by biological (age, gender, inflammatory factors,…), psychological (feelings of anxiety, depression,…) and social (loneliness, social support,…) factors.
The above explanation is completely correct and understandable for most people. It is therefore nice when physiology is made understandable. Unfortunately, this explanation can be considered as a simplification of reality. How pain is created and maintained is extremely complex. If your nervous system would be able to hear this explanation of how it presumably works, it might feel insulted by the simplicity. The complexity might also be the reason that we still do not currently have an effective treatment available for the people who deal with pain on a daily basis. We find this complexity not only in the evaluation and treatment of pain, but also in the way in which pain arises. As a person in pain, but also as a clinician, we hope to be able to provide a cause, a diagnosis or a treatment from a biopsychosocial point of view. Unfortunately, this fails just too often.
Multiple researchers and clinicians have attempted to portray this complexity in an image. Below are three images that portrays this phenomenon quite well, each in their own way.
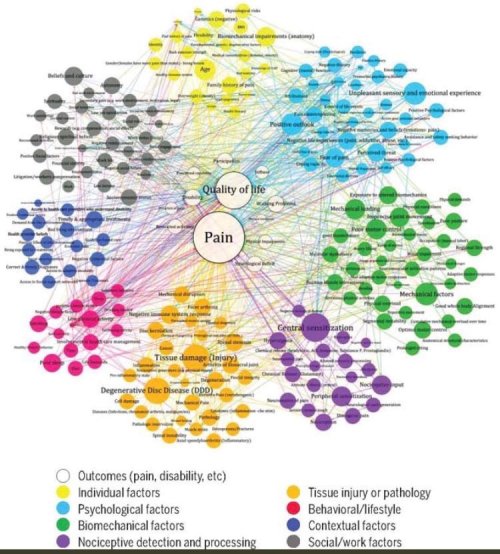
With permission of Prof. Jacek Cholewicki from Cholewicki et al. 2019 (JOSPT)
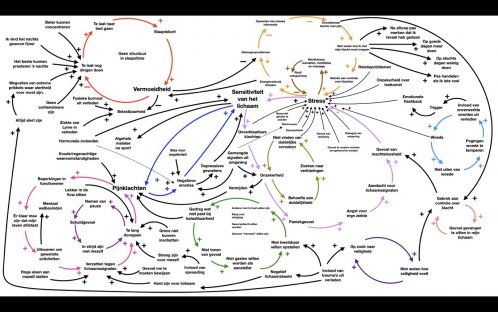
With permission of Evert Jan Das (@Everdojuan)
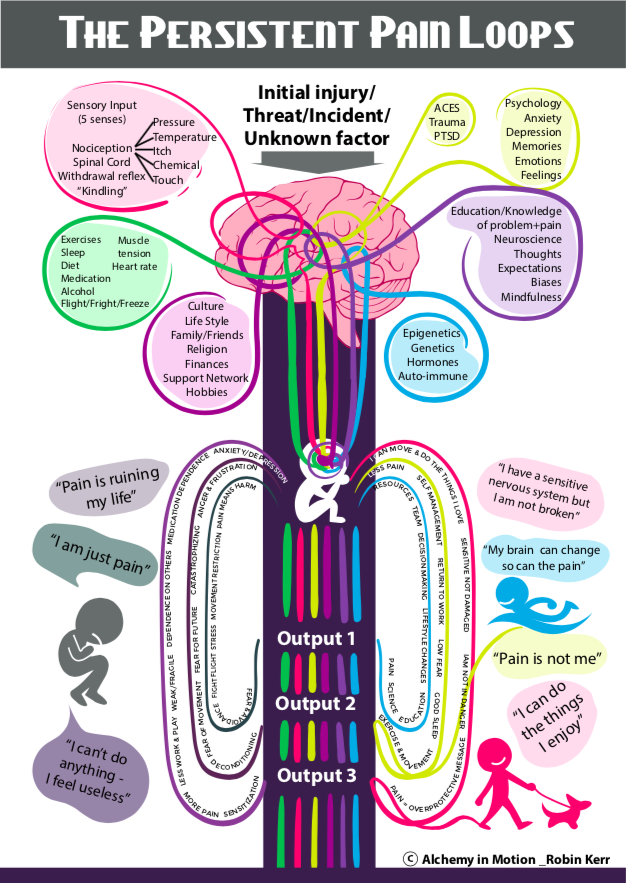
With permission of Robin Kerr.
As a researcher, clinician, or patient, it is of course frustrating to hear that something you are researching, treating or suffering from is very complex, and that we don't really know everything about it just yet. Logically, this creates uncertainty for all parties. Uncertainty is something that we as humans cannot deal with well, which is why we also like to think causally or we prefer things 'simple'. This is also reflected in the still persistent myths surrounding the origin (and treatment) of (back/neck) pain. A myth that is still very much alive is that poor posture or flexibility causes back or neck pain, even though posture and flexibility have little to do with the development of back or neck pain.
In order to maneuver in the uncertain world of pain, it is very important to recognize and accept (y)our limitations as a researcher or clinician. We do need to work with what we have (medication, movement, psychological interventions, physiotherapy,…) and not throw out all the babies with the bathwater. Also, recognize the things that we do know for sure, or that we can do well, such as not only asking for a pain score, but also actively listening and validating.
If you are new to this blog, definitely check out following blogposts which connect nicely with this one: the power of empathy, 10 do’s and don’ts for patients and self-efficacy.
Vincent Haenen
